Apex Blog
Long Term Care Still Breaks The Hearts Of Clients And Their Significant Others Trying Desperately to Open Their Claims in 2023.
Millions of Dollars are lost to this unregulated Program that continues to leave families I work with crying and overwhelmed by the bureaucracy of denial.
For most of my clients the article below by The New York Times clearly states the continuing problem.
Aged, Frail and Denied Care by Their Insurers
March 26, 2007
CONRAD, Mont. — Mary Rose Derks was a 65-year-old widow in 1990, when she began preparing for the day she could no longer care for herself. Every month, out of her grocery fund, she scrimped together about $100 for an insurance policy that promised to pay eventually for a room in an assisted living home.
On a May afternoon in 2002, after bouts of hypertension and diabetes had hospitalized her dozens of times, Mrs. Derks reluctantly agreed that it was time. She shed a few tears, watched her family pack her favorite blankets and rode to Beehive Homes, five blocks from her daughter’s farm equipment dealership.
At least, Mrs. Derks said at the time, she would not be a financial burden on her family.
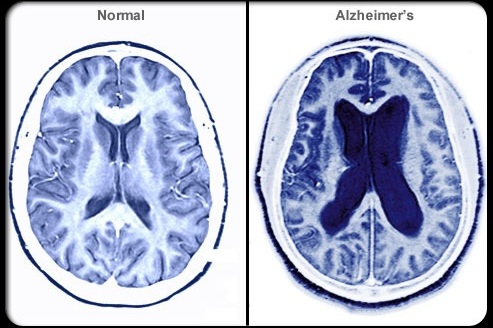
But when she filed a claim with her insurer, Conseco, it said she had waited too long. Then it said Beehive Homes was not an approved facility, despite its state license. Eventually, Conseco argued that Mrs. Derks was not sufficiently infirm, despite her early-stage dementia and the 37 pills she takes each day.
After more than four years, Mrs. Derks, now 81, has yet to receive a penny from Conseco, while her family has paid about $70,000. Her daughter has sent Conseco dozens of bulky envelopes and spent hours on the phone. Each time the answer is the same: Denied.
Tens of thousands of elderly Americans have received life-prolonging care as a result of their long-term-care policies. With more than eight million customers, such insurance is one of the many products that companies are pitching to older Americans reaching retirement.
Yet thousands of policyholders say they have received only excuses about why insurers will not pay. Interviews by The New York Times and confidential depositions indicate that some long-term-care insurers have developed procedures that make it difficult — if not impossible — for policyholders to get paid. A review of more than 400 of the thousands of grievances and lawsuits filed in recent years shows elderly policyholders confronting unnecessary delays and overwhelming bureaucracies. In California alone, nearly one in every four long-term-care claims was denied in 2005, according to the state.
“The bottom line is that insurance companies make money when they don’t pay claims,” said Mary Beth Senkewicz, who resigned last year as a senior executive at the National Association of Insurance Commissioners. “They’ll do anything to avoid paying, because if they wait long enough, they know the policyholders will die.”
In 2003, a subsidiary of Conseco, Bankers Life and Casualty, sent an 85-year-old woman suffering from dementia the wrong form to fill out, according to a lawsuit, then denied her claim because of improper paperwork. Last year, according to another pending suit, the insurer Penn Treaty American decided that a 92-year-old man had so improved that he should leave his nursing home despite his forgetfulness, anxiety and doctor’s orders to seek continued care. Another suit contended that a company owned by the John Hancock Insurance Company had tried to rescind the coverage of a 72-year-old man when he was diagnosed with Alzheimer’s disease four years after buying the policy.
In court filings, all three companies said the denials had been proper. They declined further comment on the cases, though Bankers Life and John Hancock eventually settled for unspecified amounts.
In general, insurers say criticisms of claims-handling are unfair because most policyholders are paid promptly and some denials are necessary to root out fraud.
In a statement, Conseco said the company “is committed to the highest standards for ethics, fairness and accountability, and strives to pay all claims in accordance with policy contracts.” Penn Treaty said in a statement, “We strive to treat all policyholders fairly, and to deliver the best, most efficient evaluation of their claim as possible.”
But policyholders have lodged thousands of complaints against the major long-term-care insurers. A disproportionate number have focused on Conseco, its affiliate, Bankers Life, and Penn Treaty. In 2005, Conseco received more than one complaint regarding long-term-care insurance for every 383 such policyholders, according to data from the insurance commissioners’ association. Penn Treaty received one complaint for every 1,207 long-term-care policyholders. (The complaints touch on a variety of topics, including claims handling, price increases and advertising methods.)
By comparison, Genworth Financial, the largest long-term-care insurer, received only one complaint for every 12,434 policies.
Conseco is among the nation’s largest insurers, collecting premiums worth more than $4.2 billion in 2006, of which long-term-care policies contributed 21 percent. Penn Treaty focuses primarily on long-term-care products and collected premiums of about $320 million in 2004, the last year the company filed an audited annual report.
In depositions and interviews, current and former employees at Conseco, Bankers Life and Penn Treaty described business practices that denied or delayed policyholders’ claims for seemingly trivial reasons. Employees said they had been prohibited from making phone calls to policyholders and that claims had been abandoned without informing policyholders. Such tactics, advocates for the elderly say, are becoming common throughout the industry.
“These companies have essentially turned their bureaucracies into profit centers,” said Glenn R. Kantor, a California lawyer who has represented policyholders.
Yet these concerns have been ignored by state regulators, advocates say, and have gone unnoticed by federal lawmakers who recently passed incentives intended to promote purchases of long-term-care policies, in the hopes of forestalling a Medicare funding crisis.
Conseco and Bankers Life “made it so hard to make a claim that people either died or gave up,” said Betty J. Hobel, a former Bankers Life agent in Cedar Rapids, Iowa.
“When someone is 70 or 80 years old,” she said, “how many times are they going to try before they just give up?”
A Race to Sell Policies
When Mrs. Derks bought her long-term-care policy from a door-to-door salesman in 1990, she was unaware that she represented the insurance industry’s newest gold mine.
Her husband had died eight years earlier of a stroke, leaving her to run a barley farm in northern Montana, where she lived with her three children and her aging mother. As she watched her own parent decline, Mrs. Derks became preoccupied with sparing her children the expense of her final years.
“She was terrified that she would bankrupt us or get sent to a public nursing home,” said Ken E. Wheeler, her son-in-law.
At the time, long-term-care policies, which can cover the costs of assisted-living facilities, nursing homes and at-home care, were becoming one of the insurance industry’s fastest-growing products. Companies like Conseco, Bankers Life and Penn Treaty were aggressively signing up clients who were not in the best health at rates far below their competitors’ in order to win more business, former agents said. From 1991 to 1999, long-term-care sales helped drive total revenue gains of roughly 500 percent each at Penn Treaty and Conseco, including its affiliate Bankers Life.
Cracks in the business, however, soon started to appear. Insurance executives began warning they had underestimated how long policyholders would live after entering nursing homes. The costs of treating Alzheimer’s, Parkinson’s and diabetes ballooned.
As insurers began realizing their miscalculations, they persuaded insurance commissioners in California, Pennsylvania, Florida and other states to approve price increases of as much as 40 percent a year.
By 2002, Conseco’s long-term-care payouts exceeded revenue. Those and other disappointing results prompted the company to file for bankruptcy, from which it emerged 10 months later.
That same year, Mrs. Derks entered Beehive Homes, a cheery, 12-bed center one block from the Prairie View elementary school. In the previous four years, she had been hospitalized more than two dozen times. She had once lain unconscious in her living room for a day and a half. Her physician ordered her into an assisted-living center.
Initially, Conseco told Mrs. Derks’s daughter, Jackie Wheeler, that her claim would go through smoothly, Mrs. Wheeler said. The family began paying Beehive Homes’s $1,900 monthly fee.
But three months after submitting her claim, Mrs. Derks received a letter from Conseco saying she had waited too long, and her earliest costs would not be reimbursed. Two months later, she received another letter denying her entire claim because she had not submitted proof of illness.
Yet a copy of Mrs. Derks’s policy, sent to the Wheelers by Conseco in 2004 and reviewed by The Times, mentions no requirement for proof of illness. The policy requires only that the confinement be ordered by a physician, and it allows for a notice of claim to be sent “as soon as reasonably possible.”
Mrs. Derks’s daughter called Conseco and explained that her mother could not recall the date or people’s names and had started multiple fires by forgetting to turn off the stove. She sent letters stating that her mother needed assistance to dress, eat, go to the bathroom and inject insulin.
“This is medically necessary!!!” reads a form signed by Mrs. Derks’s physician in 2004. “This has been filled out three times! This person needs assistance!”
Conseco denied long-term-care payments for Mary Derks, who has early-stage dementia, hypertension and diabetes. She bought the policy to avoid burdening her family, but it sold part of its farm-equipment dealership to pay for her care.Credit...Anne Sherwood for The New York Times
Seven months later, Conseco sent another letter, this time denying Mrs. Derks’s claim because her policy “requires a staffed registered nurse 24 hours per day.” Her policy does not mention such a requirement.
Conseco also sent letters denying Mrs. Derks’s claim because her policy had an “assisted living facility rider,” and because Mrs. Derks “does not have an assisted living facility rider.” In all, the family received more than a dozen letters from the company. Many contradict one another, and frequently cite requirements that are nowhere mentioned in Mrs. Derks’s policy.
“There was always a new step in the runaround,” Mrs. Wheeler said. “It felt like everything was designed to make me just go away.”
Over two years, Mrs. Wheeler estimated, she called the company about 100 times. Twice a month, she sent envelopes stuffed with medical records. Some afternoons, she spent hours making calls. After one conversation, Mrs. Wheeler slammed down the phone and started to cry. Then she drove to Beehive Homes, where her mother was surrounded by faded photos of her childhood and boxes of adult diapers.
“I wouldn’t tell her about the problems we were having with Conseco, because I knew it would cause her so much worry,” Mrs. Wheeler said.
Eventually, the Wheelers sold part of their John Deere dealership to raise money to pay for her mother’s care. In October 2006, they sued.
Conseco, asked by a reporter about the company’s handling of the Derks claim, declined to answer, citing the pending litigation. In court documents, the company denied Mrs. Derks’s allegations without specifying why her claim was denied.
“We did everything they asked,” Mrs. Wheeler said. “And this company just treats us like dirt.”
Tales of Bureaucracy
Inside the large Conseco headquarters in Carmel, Ind., scores of employees receive the flood of documents and calls that arrive each day. At times, according to depositions and interviews, that deluge became so overwhelming that documents were lost, calls went unreturned and mistakes occurred.
Some employees describe vast mailrooms where documents appear and disappear. One call-center representative said he was afforded an average of only four minutes to handle each policyholder’s call, no matter how complicated the questions. Employees said they were instructed not to say when the company was behind in processing paperwork, even when the backlog extended to 45 days. Workers were prohibited from contacting each other by phone, although such calls might have quickly resolved obstacles, according to depositions.
Conseco, asked in detail about the company’s policies, declined to respond.
Bureaucratic obstacles were pervasive, according to interviews with 10 former Conseco employees and depositions of more than a dozen others. Robert W. Ragle, a former Bankers Life branch manager, once contacted the claims department on behalf of a client, and “they just laughed us off the phone,” he said. “Their mentality is to keep every dollar they can.” Mr. Ragle was dismissed by Bankers Life in 2002. He sued for wrongful termination and settled out of court.
In lawsuits, complaints and interviews, policyholders contend that Conseco, Bankers Life or Penn Treaty denied claims because policyholders failed to submit unimportant paperwork; because daily nursing notes did not detail minute procedures; because policyholders filled out the wrong forms after receiving them from the insurance companies; and because facilities were deemed inappropriate even though they were licensed by state regulators.
In depositions conducted on behalf of angry policyholders, Conseco employees described bureaucratic obstacles that prevented payment of claims. Those depositions were sealed in settlement agreements but were obtained by The Times.
In a 2006 deposition, a Bankers Life and Conseco claims adjuster, Teresa Carbonel, testified that she denied claims because of missing records but was prohibited from calling nursing homes or physicians to request the documents. She also testified that when a claim was denied, she was forbidden to phone a policyholder, but instead used a time-consuming mailing system.
Ms. Carbonel’s testimony, recorded during lawsuit on behalf of a 94-year-old policyholder, Rhodes K. Scherer, also disclosed that if policyholders did not mail requested documents within 21 days, Conseco might abandon their claim, sometimes without informing them.
In the case of Mr. Scherer, who was institutionalized after a bathroom fall, it was difficult to obtain a response, Ms. Carbonel said, because the company’s requests were mailed to his home address, rather than the nursing center where the company had been notified that he had moved. Ms. Carbonel, who is no longer with the company, did not return calls. Conseco declined to comment on her testimony.
In another deposition, Conseco’s then-senior manager for long-term- care claims, Jose S. Torres, testified that Conseco would sometimes withhold payments until it received documents not required by customers’ policies. In Mr. Scherer’s case, Mr. Torres said, the company refused to pay his nursing home costs unless he sent copies of the home’s license, payment invoices and medical records, even though those documents had no bearing on approving his claim.
Mr. Scherer’s claim “was handled not in the best way, but it was handled according to the processes and procedures placed at the time,” Mr. Torres testified. “Mistakes are going to be made, you know.”
Other executives testified that when Conseco appeared to have lost important documents in Mr. Scherer’s claim, no investigation was initiated. Shawn Michael Schechter, a Conseco claims supervisor who left the company in 2005 on positive terms, according to the deposition, testified that the handling of Mr. Scherer’s claim violated the principle of good faith, which requires insurance companies to treat customers fairly.
“The claim adjuster could have made that very easy and not have put the burden back onto the policyholder,” he testified.
Mr. Torres did not return calls. Mr. Schechter declined to answer questions.
Mr. Scherer died in 2004 without receiving benefits from Conseco. His estate settled with the company in February for an undisclosed amount, according to a lawyer representing the estate.
Conseco declined to discuss its complaint history or individual cases, citing confidentiality agreements. In its statement, the company said that in 2006, Conseco paid nearly $2.3 billion on 9.8 million claims in all types of insurance sold by the company.
The company added: “Conseco, through training, education and process improvements in all of its insurance companies, is continuously focused on enhancing service and resolving any problems expeditiously. The Conseco Insurance Group’s overall insurance department complaints decreased 20 percent from 2005 to 2006.”
Depositions of executives at Penn Treaty also point to questionable practices. In a 2005 lawsuit, a Penn Treaty senior vice president, Stephen Robert LaPierre, testified that the company rejected one claim without informing the policyholder why, asked for information that was not required to process a claim, gave incomplete information about a claim’s status and said the company was delaying payment because of an investigation while failing to take steps that might have resolved the inquiry.
Mr. LaPierre declined to discuss his testimony. Penn Treaty settled the lawsuit by paying the policyholder an unspecified amount, the policyholder’s lawyer said.
Penn Treaty said in a statement that evaluating a company by measuring its complaints was flawed, and that since 2003, the company has denied an average of less than 1.7 percent of the up to 8,000 claims it received every year because of reasons related to policyholder eligibility. “From time to time, Penn Treaty is compelled to investigate fraud or questionable billing activities,” the company added.
Few Regulatory Inquiries
Few of the cases or complaints filed against Conseco, Bankers Life, Penn Treaty or other insurers have received much attention, in part because many lawsuits filed against long-term-care insurers have been settled with the requirement that depositions, documents and settlement terms be kept confidential. Frequently, say policyholders’ lawyers, the companies have been willing to pay millions of dollars in exchange for confidentiality.
Furthermore, despite the complaints against long-term-care insurers, few states have conducted meaningful investigations.
Ron Gallagher, a deputy commissioner with the Pennsylvania Insurance Department, said, “I don’t know that we have a real problem with improper claim denials.”
Yet data from the National Association of Insurance Commissioners show that from 2003 to 2005, Pennsylvania received more complaints regarding Conseco, Bankers Life and Penn Treaty than any other state. Mr. Gallagher said he might begin a new review of those companies.
Other states with large numbers of long-term-care complaints, including California, Missouri, Maryland, Indiana and Washington have not begun investigations, or have reviewed only small numbers of policies.
As a result, other seniors may end up like Mrs. Derks.
While she was waiting for her lawsuit to proceed, Medicaid began contributing to Ms. Derks’s care. Taxpayers now pay Beehive Homes about $32 daily for her care.
“Long-term-care insurance is supposed to result in less pressure on Medicaid, not more,” said Ms. Senkewicz, the former executive at the insurance commissioners’ association.
For Mrs. Derks’s family, things have already broken down.
“How many other people are out there who don’t have a family to fight for them and have just given up?” asked Jackie Wheeler. “This company should be ashamed.”
What to do when you fall…